Genetic Testing For All: Is It Eugenics?
 In recent weeks, there’s been talk of three types of genetic testing transitioning from targeted populations to the general public: carrier screens for recessive diseases, tests for BRCA mutations, and non-invasive prenatal testing (NIPT) to spot extra chromosomes in fetuses from DNA in the maternal bloodstream.
In recent weeks, there’s been talk of three types of genetic testing transitioning from targeted populations to the general public: carrier screens for recessive diseases, tests for BRCA mutations, and non-invasive prenatal testing (NIPT) to spot extra chromosomes in fetuses from DNA in the maternal bloodstream.
Are these efforts the leading edge of a new eugenics movement? It might appear that way, but I think not.
When I began providing genetic counseling 30 years ago at CareNet, a large ob/gyn practice in Schenectady, NY, few patients were candidates for testing: pregnant women of “advanced maternal age” (35+), someone with a family history of a single-gene disorder or whose ethnic background was associated with higher prevalence of a specific inherited disease. Their risks justified the cost and potential dangers of the tests.
Now the picture is rapidly changing as plummeting DNA sequencing costs and improved technologies are removing economics from the equation. It’s becoming feasible to test anyone for anything – a move towards “pan-ethnic” genetic screening that counters the “sickle-cell-is-for-blacks and cystic-fibrosis-is-for-whites” mindset.
So here’s a look at three very different types of genetic tests that are poised to make the leap to the general population. And despite new targets revealed with annotation of human genomes, some of the detection technologies themselves are decades old.
 #1: CARRIER SCREENING
#1: CARRIER SCREENING
Population screening for carriers of single-gene diseases has been around since those for sickle cell disease and Tay-Sachs disease in the early 1970s. We learned a lot from their starkly different results. For years, labs such as Athena Diagnostics, the Baylor College of Medicine Medical Genetics Laboratories, Emory Genetics Laboratory, Ambry Genetics, GeneDx and others have added genetic tests to their rosters, which now cover hundreds of single-gene diseases, from A (Alport syndrome) to Z (Zellweger syndrome).
Other companies have recently visited CareNet, pitching tests for more single-gene diseases for everyone. For example, Natera’s Horizon Carrier Screen tests for 39 conditions and 127 variants of the cystic fibrosis (CF) gene. They provide genetic counseling by phone, which is common these days, given the scarcity of trained genetic counselors, especially outside cities. And Natera can tailor screening panels to specific populations.
In addition to the changing economics, the public is more familiar with DNA-based tests, partly due to the direct-to-consumer testing company 23andMe. Before FDA forbade them from selling carrier tests as “information,” thousands of people learned about recessive diseases from the company’s excellent website.
Cystic fibrosis illustrates the widening of test offerings. Carrier screening began in 2001 for whites and Ashkenazi Jews, following recommendations from the American Congress of Obstetrics and Gynecology and the American College of Medical Genetics. By 2005, with many more mutations identified and the diagnosis broadened, testing expanded to everyone. At CareNet every pregnant patient gets a CF test, along with a factsheet that I wrote.
CF is just one gene of thousands. Researchers from Counsyl, another newer player, published a key paper reporting on 23,453 patients from ob/gyn, genetics, and infertility clinics screened for 108 disorders. Nearly 24% carried at least one disease-associated recessive mutation! 5.2% (1,210) carried 2 or more, and .33% (78) actually HAD a disease by having inheriting two mutations.
Interestingly, stratifying participants by population group revealed the differences that once fueled restriction of testing. Although overall 24% of the total carried at least one disease, that ranged from 6.3% among Native Americans and 8.5% among East Asians to 47.1% among the Finns and 43.6% among Ashkenazi Jews. Only 15.8% of African-Americans were carriers.
#2 BRCA TESTING FOR ALL
 Last week in a controversial Viewpoint in JAMA Mary-Claire King and colleagues suggested “that population-based screening of women for BRCA1 and BRCA2 should become a routine part of clinical practice.” These genes normally participate in DNA repair, and mutations raise risk of several cancers, not just the widely-reported breast and ovarian. (BRCA1 mutations predispose to cancers of the cervix, colon, uterus, and pancreas, and BRCA2 to cancers of the stomach, gallbladder, pancreas and bile ducts, as well as to melanoma.)
Last week in a controversial Viewpoint in JAMA Mary-Claire King and colleagues suggested “that population-based screening of women for BRCA1 and BRCA2 should become a routine part of clinical practice.” These genes normally participate in DNA repair, and mutations raise risk of several cancers, not just the widely-reported breast and ovarian. (BRCA1 mutations predispose to cancers of the cervix, colon, uterus, and pancreas, and BRCA2 to cancers of the stomach, gallbladder, pancreas and bile ducts, as well as to melanoma.)
Results from the first families that Dr. King analyzed, published in 1990, were Ashkenazi Jewish with several affected members, because it is easier to discover a gene and what it does in a population with very few variants. It turned out that this group has only three mutations, all of which obliterate the genes’ vital function. Sequencing the entire huge gene wasn’t necessary, lowering costs substantially.
Based on the 1990 paper and follow-up, for years we genetic counselors would consider the number of cases of the relevant cancers and ages at diagnosis in families. We used published guidelines to decide to whom to offer BRCA testing.
That approach invariably missed some cases in families that were small or had few female members. We knew that accruing data on populations beyond the high-risk Ashkenazim would take years, mostly because thousands of mutations exist.
Many people thought Dr. King’s suggestion of wider BRCA screening premature. Criticism centered on the experimental design in the PNAS paper that the Viewpoint addressed, also from the King group. It focused on Ashkenazim because with fewer mutations the data were easier to collect, especially back when the study began.
The researchers tested more than 8,000 healthy Ashkenazi men in Israel for BRCA1 and BRCA2 mutations, and then offered testing to all female relatives of the 175 men found to have mutations. These women, it turned out, indeed had very high risks of developing the associated cancers – and about half of them had NO family history. Following the old guidelines would have missed them. (An important caveat in the Viewpoint cautioned that testing should only be for meaningful mutations – not the many “variants of uncertain significance.”)
But we can’t know which mutations lurk in whom unless we look for them! And not testing members of families that don’t fit the original pattern will miss cases. That’s what happened in my friend’s family.
Maya’s son discovered he had a BRCA mutation after he took a 23andMe test, for fun, back when one could do this. Maya was tested next because she’s Ashkenazi, but it was her husband, who’s Catholic and European, who’d passed on the mutation to their son. Fortunately their daughter escaped the family legacy. But here’s a family in which the cancer can indeed begin in either father or son, and in more distant relatives. The affected individuals are now being tested regularly for the associated cancers – no one is running off to have organs removed. A positive genetic screen result — meaning identification of a gene variant, not a diagnosis — signals a need for vigilence and preventive health care. It’s not a ticket to surgery.
#3 FETAL DNA TESTING
Until recently, testing fetal DNA (NIPT) was only advised for pregnant women at higher risk of the fetus having an extra chromosome 13, 18, or 21, the most common trisomies. That is, women over 35, or who’d had a previous trisomy. Soon it will be offered to all.
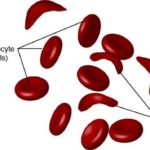
Entire fetal genomes can be sequenced from DNA snippets in the maternal bloodstream, which are shorter than the woman’s DNA pieces. But whole genomes are, for now, TMI. The first commercial non-invasive fetal DNA tests detect abnormal chromosome ratios or differences at single sites (SNPs) on those chromosomes in both genomes, in high-risk women. By August 2014, the data indicated that NIPT is safe enough for low-risk women.
At least half a dozen companies now offer NIPT. It will clearly save lives.
“The sweet spot is for women who are deciding whether or not to have an invasive procedure because they are at higher risk due to advanced maternal age, a positive screen of serum markers, or a fetal sonographic abnormality. If testing fetal DNA gives an all-clear, at least for these three chromosomal conditions, then the pregnant woman can avoid the risk of a more invasive procedure, such as amniocentesis,” Diana Bianchi, MD, professor of pediatrics at Tufts University, told me.
Dr. Bianchi is the mother of the invention, described in this DNA Science blog post. She reported detecting cell-free fetal DNA and suggested noninvasive prenatal testing back in 1996. “Nine to one, women want the blood test first, and a great majority of them have a negative result, so they don’t go on to have amnio or CVS,” she added.
But that benefit wasn’t immediately obvious to critics unfamiliar with the spectrum of prenatal testing options. Dr. Bianchi received threats from people who saw testing fetal DNA as a way to avoid the births of people with Down syndrome and the other trisomies.
 IS IT EUGENICS?
IS IT EUGENICS?
Eugenics is “the science of improving a human population by controlled breeding.” Mention of the term is often followed by reference to Nazis.
Are recessive disease carrier screening, BRCA mutation testing, and NIPT eugenic, according to the definition? Only one might be, and even that’s questionable. Let’s dismiss the other two first.
BRCA testing alerts relatives to the need for active surveillance for certain cancers, for their own health. At least in my experience in counseling patients, an inherited cancer susceptibility is not a reason to keep one person from having kids with another, or to end a pregnancy, because the cancers are late-onset and treatable. Plus, a person who inherits a BRCA mutation must then undergo a second, somatic mutation in a cell in the organ that develops cancer, according to the classic two-hit mechanism. It isn’t the cancer that’s inherited, but the increased risk.
NIPT is not eugenic in its current guise because trisomies – extra chromosomes – result from mispairing in meiosis. They’re not inherited, they just happen, although a person with a trisomy is more likely to produce “unbalanced gametes” that can perpetuate the situation. But most new trisomies are spontaneous glitches that result from a chromosome pair not parting when it should as sperm or egg form.
The one type of testing that could ultimately have a eugenic effect is carrier screening for recessive diseases. The Counsyl paper concludes that “sequencing the entire genome of each patient would reveal ~10 times as many lethal recessives on average.”
Imagine including one’s personal collection of recessive mutations on a DNA dating site! (See yours truly quoted in The New Science of Matchmaking: Dating Based on Your DNA).
Natera’s description of the Horizon Carrier Screen leads potential patients through Mendel’s first law: an offspring of two carriers of the same condition faces a 25% chance of inheriting the disease. “If you find you are at risk, you can take steps to prevent having a baby with a genetic disease,” the clear explanation continues.
For couples who discover they carry mutations in the same gene, the company offers Spectrum, which uses pre-implantation genetic diagnosis (PGD) to choose embryos conceived in vitro that have not inherited the disease-associated genotype. PGD has been around since 1990, but occasionally headlines trumpet it as new.
So yes, filtering out mutations with rigorous and actionable carrier tests can ultimately alter the gene pool. And because the selection is directional, this appears to be eugenic by permitting only certain gene variants into the next generation. But this isn’t really eugenics, because the important descriptor of eugenics is INTENT; that of medical genetic screening and testing is CHOICE. The goal of the first is sociological, the second, biological.
Genetic screening and testing often aim to avoid a medical situation in a family, not to “improve” the genetic structure of a future population. And we should never assume that all families will choose that path. I’ve talked to families that have more than one child with spinal muscular atrophy, or with a blood disorder, because preventing the birth of another affected child may seem a rejection of the beloved existing one. (See the DNA Science posts about the Amish for more examples.) Families must be allowed that choice. That’s what genetic counseling is all about.
And so I don’t think that any medical genetic screening or testing is eugenic, and I welcome the coming expansion of the opportunity to learn what’s in some of our DNA to more people.




Great to see this topic getting media coverage – we need more discussion in the public domain about these issues.
I do however have some reservations about this perspective. I think the question is not about eugenics, especially when narrowed to the definition given in this article, it would be more useful to be asking whether our society considers it an ethical practice. I find it interesting that the rhetoric around prenatal genetic counselling always emphasises that it is a woman’s choice to test and yet here we have a counselling service that routinely tests all patients for CF carrier status – what happens to couples who don’t want to know? I also think it interesting that the emphasis in this article seems to be about the high carrier rate for recessive disease, but there is no mention of the enormous variation in the severity of some of these diseases. If patients are given the opportunity to make an informed decision about carrier testing they need information about the condition as well as knowing their risk of being a carrier. For some families their perception of the severity of a condition will influence their decision more than their risk of being a carrier.
The introduction of screening all pregnant women with NIPT is of particular concern and differs from BRCA and prenatal carrier screening in that it can only be offered to women who are already pregnant whilst the other tests can be offered pre-pregnancy. When testing is offered during pregnancy there are only two options if a positive result is received – continuation or termination of the pregnancy. This is an ethical minefield for many couples and cannot be compared to the relative simplicity of deciding on whether to know BRCA status which might entail taking preventative action. We need to ensure that the ethical issues surrounding prenatal testing do not get lost in the general debate about population genetic screening.
Thanks Marleen for the several important points that you raise. Many ob/gyn practices here in the US offer CF carrier tests. I wrote a FAQs that describes the phenotypes associated with several allele combinations for the patients, and any patient is free to meet with me to learn more, at no extra cost. Patients can opt out of any test. Of course you are correct that full informed consent for massive carrier screening would be difficult, and the practice I counsel for has in fact turned down those company pitches.
Several past posts have dealt with the bioethics (https://blogs.plos.org/dnascience/2012/10/18/prenatal-genetic-testing-when-is-it-toxic-knowledge/) of genetic testing . I wanted to compare techniques and bring up eugenics, which is so much longer-term and not discussed as much.
Thanks for posting!