Mitohype: 3-Parent Designer Babies Who Will Change Human Evolution
 If I turned in a 20,337 word article and the editor decided to replace 37 of those words, would I call her a co-author? Certainly not. So why does replacing 37 genes in a fertilized ovum destined to develop into a sick child conjure up images of ménages-a-trois in Petri dishes and mingling chromosomes? Those genes, most of which control energy metabolism, are delivered in mitochondria that replace their mutation-bearing counterparts.
If I turned in a 20,337 word article and the editor decided to replace 37 of those words, would I call her a co-author? Certainly not. So why does replacing 37 genes in a fertilized ovum destined to develop into a sick child conjure up images of ménages-a-trois in Petri dishes and mingling chromosomes? Those genes, most of which control energy metabolism, are delivered in mitochondria that replace their mutation-bearing counterparts.
To read some of the media coverage a week ago, you’d think that the February 25th meeting of the Cellular, Tissue, and Gene Therapies Advisory Committee at the Food and Drug Administration (FDA) was to discuss creating monsters, not manipulating mitochondria. But it’s not really the media’s fault. One of the researchers who spoke at the session recently published a technical article entitled “Three-parent in vitro fertilization: gene replacement for the prevention of inherited mitochondrial diseases,” so I suppose some mitohype is to be expected.
ETHICAL OBJECTIONS
I listened to the first day of the FDA meeting on assignment for Medscape. The focus was the state of the science that might or might not support approval of a phase 1 safety clinical trial of mitochondrial replacement. Several experts told of their preclinical work, on human cells and embryos of mice, cows, and monkeys, and the day wrapped with discussion by the FDA committee, which includes clinicians, scientists, and bioethicists. But in between was a session of public comment.
Two approaches are being considered: introducing the male and female nuclei from a fertilized ovum into an egg from a healthy donor that presumably contains healthy mitochondria, and “spindle transfer,” which uses the apparatus that divides chromosomes to deliver the mitochondria that naturally gather around it to power cell division. (Recall from 10th grade biology that a mitochondrion is “the powerhouse of the cell.”)
I found it odd that bioethics wasn’t on the FDA’s agenda, but thought perhaps the technology would be deemed too soon or off limits based on the science alone. I expected that the public commentators might be from families with mitochondrial diseases, but to my surprise the 7 speakers focused on bioethics.
A statement earlier in the month from the Center for Genetics and Society that appeared, in part, in the previous Sunday New York Times as “Genetically Modified Babies” set the tone. While I agree with the statement’s conclusions that “more than 250 signatories” endorsed that the technology simply isn’t necessary, it included the sort of inflammatory language that has plagued the modern biotech industry from the start in the 1970s. Listening to the public comments, after a morning of experimental details involving spindles, mitochondria, and pronuclei, the switch to research described as “authorized intentional genetic modification of children and their descendants” might have been literally accurate, but I found it jolting and seemingly missing the intent and extent of the technology.
Although some of the public comments addressed mitochondrial manipulation, for the most part they veered down that oft-evoked slippery slope to clones and bizarre vegetables. Here are a few:
“Who is the mother? One cell is just getting a couple dozen mitochondrial genes, but the woman’s egg that is enucleated is getting 20,000 genes. The new individual is the product of a massive procedure, like a genetically modified tomato. This new individual is a genetically modified human being.” (Hank Greely’s “Heather Has Three Parents” at the Law and Biosciences Blog from Stanford Law School points out that our genomes are modified, quite naturally, all the time.)
“It is a gateway technology to use SCNT (somatic cell nuclear transfer) or other methods in human trials. We need to look more carefully at animal research on cloning.” (The FDA discussion was on manipulating oocytes, not somatic cells. But cloning was mentioned so often that I was reminded of the old marijuana-leads-to-heroin argument. And nuclear transfer has been around since the 1960s, to clone non-human animals.)
“This biotechnology could alter the human species.” (Health care routinely alters evolution of our species.)
One otherwise eloquent speaker uttered the following so fast I could barely keep up. She had “Grave concerns” about the “creation of GM children,” “perversion of the relationship between parents and children,” “alteration of the human species,” and “GATTACA-like classes of human beings and the dissolution of our humanity.”
And finally, “we all remember Jesse Gelsinger,” said a prominent speaker gravely. Indeed we do. Jesse was 18 years old when he died following a gene therapy procedure, as I discuss in depth in my book on that biotechnology. Although Jesse Gelsinger was once a fertilized egg, he was never an oocyte, the subject of discussion. I think the point was informed consent.
The emotion and hyperbole perhaps weren’t necessary. As more than one committee member pointed out, it was an astute FDA scientist (Frances Oldham Kelsey, MD) who averted a thalidomide disaster in the U.S. back in the early 1960s.
As we await further public comment, possible until May 9, here’s some interesting facts about mitochondria that didn’t make it into most news coverage.
COOL THINGS ABOUT MITOCHONDRIA
Gerald Shadel, PhD, director of pathology research at the Yale School of Medicine, delightfully opened the morning session introducing mitochondria as “double-membraned submarines that cruise around cells but are actually very complex, forming large elaborate dynamic networks.” The biology of these cell parts is highly unusual, and that’s perhaps why the public discussion kept returning to the more familiar cloning. But a mitochondrion has nothing much in common with a cloned somatic cell.
THE ENDOSYMBIONT THEORY Mitochondria look like bacteria, reproduce like bacteria by growing and splitting, and have their own DNA like bacteria. That’s because they likely descended from bacteria that were presumably swallowed up by the earliest complex cells. Today mitochondria are integrated parts of ourselves — the energy reactions that they house also require expression of genes from the nucleus.
MATERNAL INHERITANCE Eggs are packed with lots of stuff, including many mitochondria. Not so the streamlined sperm, whose mitochondria cling to its midpiece section, ready to fuel the long swim to the egg. Should an errant mitochondrion sneak into a sperm head and survive the cervical journey and make it into an egg, maternal molecules soon dismantle it. Meanwhile, most of the 1 in 200 eggs that have a mitochondrial mutation stop developing. Isn’t the female body amazing?
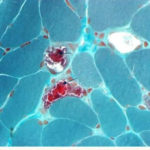
UNPREDICTABLE VARIABILITY Body (somatic) cells have 2 copies of each chromosome, and therefore 2 copies of each gene. But cells have many mitochondria, especially skeletal muscle cells, which can have thousands. That’s why a mitochondrial disease often causes great fatigue and weakness.
A mitochondrion has several copies of its tiny genome, each one a mere 16,569 DNA nucleotides, compared to the 3 billion or so in the nucleus. The genetic landscape of the mitochondria in a cell is more a population of gene variants than the 1:1 ratio seen in a person who is a carrier (heterozygote) of a nuclear gene.
If a woman is a heterozygote for a mitochondrial gene (has two variants), as the number of mitochondria whittle down from 100,000 to about 100 as the egg matures, some eggs end up with about equal copies of each gene variant, but most are skewed, getting all healthy versions or all bad ones. This unpredictable inequality, called heteroplasmy, means that a woman can be healthy, but have a child with a mitochondrial disease when the developing egg unluckily picks up many copies of a mutation.
Heteroplasmy also means that siblings may be affected to very different degrees, that symptoms may not start until enough cells with mutant mitochondria accumulate, and that mitochondria in one cell type may be packed with the mutation but not so others, complicating diagnosis based on symptoms and testing an accessible body fluid.
 TSAR NICHOLAS II On a July night in 1918, Tsar Nicholas II of Russia and his family, the royal Romanovs, were shot, their bodies damaged with acid and buried in a shallow grave. In July 1991, two amateur historians found the grave and sent DNA samples for testing. Y chromosomes distinguished the males and mitochondrial DNA (mtDNA) identified the Tsarina and her three daughters.
TSAR NICHOLAS II On a July night in 1918, Tsar Nicholas II of Russia and his family, the royal Romanovs, were shot, their bodies damaged with acid and buried in a shallow grave. In July 1991, two amateur historians found the grave and sent DNA samples for testing. Y chromosomes distinguished the males and mitochondrial DNA (mtDNA) identified the Tsarina and her three daughters.
But probing the DNA of descendants of the royals showed that the remains thought to be the Tsar differed at base 16169 in the mtDNA from that of his living great-grandniece Xenia. The Tsar’s mtDNA had T at the site in some samples, C in others.
Before we knew much about the changeability of the mitochondrial genome – it doesn’t repair itself like nuclear DNA and is splashed with oxygen free radicals from all those energy reactions – forensics researchers thought the Tsar’s strange DNA must have been due to a sequencing error. But then in yet another July, in 1994, researchers exhumed the body of Nicholas’s brother, Grand Duke Georgij Romanov. His mtDNA at position 16169, in bone cells, also went both ways, with a T or a C.
The heteroplasmy that confused forensic analysis of the Romanovs isn’t rare after all. Sequencing of many mitochondrial genomes has revealed that one in ten bases can differ within an individual.
COENZYME Q This molecule that takes part in the reactions of cellular respiration graces the shelves of health food stores, and is in dozens of clinical trials to evaluate treatment of a wide range of neuromuscular disorders, heart disease, and reproductive uses. It’s in phase 3 clinical trials to treat mitochondrial diseases.
TROUBLESHOOTING
After the expert presentations and public comments, the FDA committee members, including scientists, physicians, and bioethicists, listed the science-based problems with mitochondrial manipulation that had emerged:
Will mixing mitochondria and eggs from two populations be a problem? Carlos Moraes, PhD. of the University of Miami Miller School of Medicine offered the example of a Brit going to Australia and marrying an aborigine to make the point that it wouldn’t.
Heteroplasmy. It happens, but in non-human animal studies hasn’t been a problem.
Carryover. How can we know if some mutation-bearing maternal mitochondria get into the manipulated fertilized ovum? If it does, will it affect health? Over time, heteroplasmy does tend to shift towards favoring one gene variant. The risk of carryover is unknown.
Could the delicate fertilized ova be damaged or lose chromosomes? Sure. That’s a risk of IVF, but preimplantation genetic diagnosis (checking a cell of an early embryo) can get around that.
Could resulting children be damaged? Possibly. IVF increases the risk of Beckwith-Wiedemann Syndrome, an overgrowth condition that predisposes to cancer. The link took years to show up because the condition hadn’t been seen in animal models.
Katharine Wenstrom MD, a clinical geneticist from the Alpert Medical School of Brown University, summed matters up. “A lot of patients don’t develop symptoms until adulthood because it takes that long for abnormal mitochondria to accumulate. This makes me nervous to talk about a healthy blastocyst being good to go, or an animal model. There are so many aspects of mitochondrial disease that we don’t understand, such as tissue specificity, changes over time, and response to environmental stimuli.”
PRACTICAL MATTERS
I heard several people mutter “adoption” during the late-afternoon discussion as an alternative to creating a fertilized ovum with healthy mitochondria. Using a donor egg is another option.
I’d wondered why members of families with mitochondrial disease hadn’t been among the public commenters. Then, at the wrap-up, Sharon Reeder eloquently and non-hysterically put everything into perspective.
“How can we prevent when we can hardly diagnose? I was diagnosed 14 years ago. It took 16 years. My first symptom, when I was 18, was a droopy eyelid. They fixed it, and nobody asked why. I had a child when I was 35 and when I was 36 I was diagnosed. Pregnancy and giving birth were incredibly hard. I ended up in a wheelchair after I gave birth. I was negative in blood but positive in a muscle biopsy. I now have 10 doctors. Healthy people don’t go in to get their mitochondria checked.
I’m sitting here thinking, ‘Oh gosh! It would be so great if I was listening to all this research and it was about therapies for those of us with mitochondrial disease, helping those of us whose lives are severely affected. But this might be the gateway to that.”
At the risk of misinterpreting Ms. Reeder, the gateway that she mentions differs from the gateway to the slippery slope that would lead from research on mitochondrial replacement to the making of designer 3-parent babies that would disrupt the parental-child bond and alter the course of human evolution forever. I think she means that even if this particular biotechnology never makes it to clinical trials – for whatever reasons – what we learn from the journey could ultimately translate into treatments based on new understanding of the tiny genomes within the still-mysterious powerhouses of the cell.

Who do people think they are in deciding to create some bizarre designed baby when NATURE plainly shows you SHOULDN’T BE BREEDING. You have unhealthy genes. This ‘It’s my right to breed like a bug or germ’ by humans is appalling and why we are destroying the planet when our numbers should be regulated than spewed out like viruses CUZ WE CAN. The genetic male imperative to breed mindlessly without regard to the environment or the species. Knowing my family’s health problems I refuse to pop out a spawn just cause. There’s not a healthy enough partner to make me rethink forcing a child into the world for my benefit and ego, and spend money to mitigate the inherent problem nature would’ve answered with a dead baby.
[…] If I turned in a 20,337 word article and the editor decided to replace 37 of those words, would I call her a co-author’ Certainly not. So why does replacing 37 genes in a fertilized ovum destined to Read full article […]
An interesting point. I did notice that for the first day I listened to of the FDA session, no one who is affected actually requested that this research be done. The lone voice from the patient community, at least she was the only one who identified herself as such, was not for it. I’m not so sure patients even want this intervention. In genetic counseling the issue you mention comes up often — some parents would do anything not to have another sick child, yet others turn down testing and termination because it seems like a rejection of the existing sick child. It is difficult to pass judgment if we are not in their shoes.
Thanks for actually reporting on the meeting. There were several pre-meeting pieces on what the FDA was considering (including, I blush to admit, one by me at the Genetic Literacy Project), but yours is the only one I’ve seen that told us about what happened. It’s an interesting point, the lack of advocates. If there isn’t an active patient community demanding cures for mitichondrial diseases, then why is the FDA even taking up its time with this topic? The agency has a ton of work to do, and it usually moves quite slowly. This sounds more and more like a bad use of its resources, including staff time to put together the extensive background materials.
Thanks Tami. I was so involved in reporting the details (and I admit to not understanding it all) that it took a few days for me to realize that there was indeed a lack of interest from the very community that this controversial research is supposed to help. You hit the nail on the head!
[…] children. More specifically, researchers have developed a method that enables mother’s to conceive children that have three unique DNA strands, which in turn will enable scientists to eliminate genes that carry a particular virus or illness […]
The diseases impacted deal with mitochondrial DNA which comes from the mother.
Glenn McGee
It does not deal with paternally induced issues at this time. Potential maladies affected could include disorders of the heart or liver, respiratory ailments and muscular dystrophy.
Glenn McGee The procedure, which can take place with an unfertilized egg or an embryo, would require material from a donor egg or embryo.Glenn McGee
Modern medicine has come a long way and if it can help eliminate the disease for mothers who want to have children is it really that bizarre and a far fetched idea? People don’t usually “pop out spawn just cuz”. They want to have a baby, a healthy one at that. And if the technology is out there we should use it